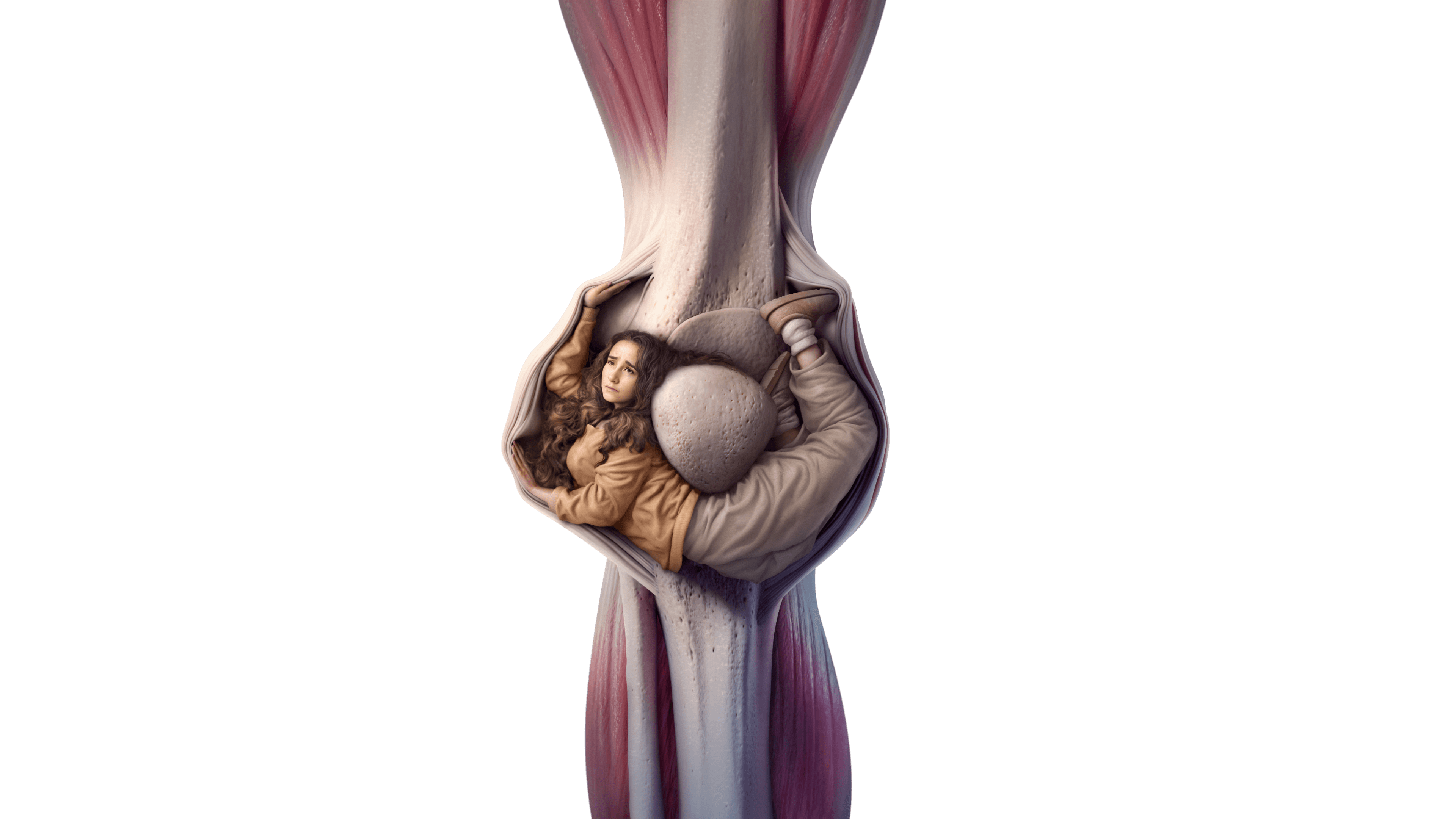
The diagnosis of tenosynovial giant cell tumor (TGCT, also known as pigmented villonodular synovitis [PVNS]) relies upon three key steps: clinical assessment, radiological evaluation and pathological analysis.1,2
TGCT diagnostic pathway: Overview
presentation

conditions*

diagnosis

evaluation

TGCT

diagnosis
Delayed diagnosis is a challenge in TGCT, with the median time from the onset of symptoms to definitive diagnosis reported to be 18 months.5
For more information about each step, including some of the current challenges, click on the drop down menus below:
The non-specific symptoms of TGCT can lead to misdiagnosis and a delay in establishing a definitive diagnosis.3
Typical clinical indicators for TGCT include:
Patients may visit many different healthcare professionals before referral to an orthopedic surgeon or oncologist3

- Subtle radiographic changes in MRI scans can make early detection difficult5
- The rarity of TGCT and gaps in understanding can also delay diagnosis3
Typical MRI presentation
CLICK D-TGCT TO FIND OUT MORE
Small, dense, well-defined nodules7,8
Image: Mastboom MJL, et al. Acta Orthop. 2017;88( 6):688-94. Available at: https://actaorthop.org/actao/article/view/9750/13407. Accessed: August 2025.
Infiltrative growth pattern; can involve muscle and subcutaneous tissue near the joint7,8
Image: Mastboom MJL, et al. Acta Orthop. 2017;88( 6):688-94. Available at: https://actaorthop.org/actao/article/view/9750/13407. Accessed: August 2025.
MRI is the preferred technique for detection and characterization of TGCT2
T2-weighted imaging and gadolinium contrast is recommended to better identify hemosiderin deposits, a hallmark of TGCT.2,6,8

X-rays and CT may fail to detect TGCT due to a limited ability to visualize the extent of lesion involvement.9
While MRI can be highly suggestive for TGCT, pathological analysis is required for a definitive diagnosis.2,3
MRI INDICATORS OF TGCT
- Hemosiderin deposits are a defining characteristic of TGCT2,8
- Location is key to TGCT, and subtype diagnosis due to TGCT’s resemblance to other soft-tissue tumor types8,10
- N-TGCT typically appear as discrete, well-defined lesions, sometimes off-center or surrounding the joint8,10
- D-TGCT is usually characterized by a more wide-spread tissue mass, with distal joint effusion8,10
D-TGCT, diffuse-type TGCT; MRI, magnetic resonance imaging; N-TGCT, nodular-type TGCT; TGCT, tenosynovial giant cell tumor.
Pathology exams provide a definitive diagnosis of TGCT.2,3
Biopsy may be avoided if radiological assessment in an expert center is highly suggestive of TGCT and resection is planned. In such cases, a pathological diagnosis will be confirmed on the surgical specimen.2
Biopsy or surgical resection
Synovial fluid and/or tissue
from
the affected joint may
be collected,
as blood in
synovial fluid may
indicate a
need for further tests4
Image source: Stacchiotti S, et al. Example of a diffuse-type TGCT (D-TGCT) consisting mostly of mononuclear cells without readily identified multinucleated giant cells, and numerous foamy histiocytes.2
Immunohistochemistry (IHC)
Giant cell-rich tumors (GCRT),
including TGCT, often exhibit
similar
morphology. In some
cases, CSF1
IHC can support the
differential
diagnosis of TGCT11
Image source: Stacchiotti S, et al. Immunohistochemistry in TGCT reveals expression of clusterin in the large mononuclear cells.2
PATHOLOGICAL INDICATORS OF TGCT
TGCT lesions typically comprise a range of different cell-types:
- Mononuclear cells2
- Osteoclast-like giant cells2
- Foamy macrophages2
- Other types of inflammatory cells2
The diagnosis and management
of TGCT raises
a number of
challenges2,3
 Click here to explore
Click here to explorethe role of surgery in
the management
of TGCT

the challenges for patients
unable to have surgery
for TGCT

 Pathological
Pathological